History: A 71-year-old healthy woman presented with non-specific right-sided abdominal pain and was subsequently found to have a right renal mass. Upon surgical removal, a firm 5.1 cm tan-yellow mass was found. It extended to the renal hilum.
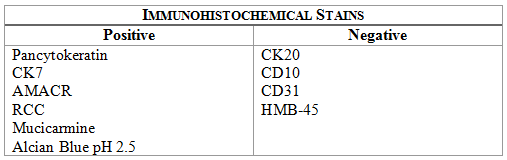
The tumor was well-circumscribed (Fig. 1a) but focally infiltrated its thin fibrous capsule (Fig. 1b). It consisted of sheets of spindled cells with vacuolated cytoplasm comprising much of the tumor (Figs. 2, 3). Bland-appearing cuboidal cells lined scattered tubular structures (Fig. 4). Histiocytes were commonly found (Fig. 5). Extracellular mucin was also present (Figs. 6a, 6b) confirmed by positive Alcian Blue pH 2.5 and mucicarmine stains. In addition, the tumor showed positive staining for pancytokeratin, CK7, AMACR and RCC (Fig. 7) with weaker focal positivity for CK34bE12. The tumor did not stain with CK20, CD10, CD31, or HMB-45.
Diagnosis: Mucinous Tubular and Spindle Cell Carcinoma (MTSCC) of Kidney
Jenny L. Smith, D.O. and Donald R. Chase, M.D.
Department of Pathology & Human Anatomy
Loma Linda University Medical center, Loma Linda, California
Discussion: In 1997, Dr. MacLennan [MacLennan et al] first described this low-grade, pleomorphic neoplasm of the kidney terming it “mucinous tubulocystic renal carcinomaâ€. He thought that it was a subset of collecting duct carcinoma, but fifteen years later, in 2002, the World Health Organization consensus conference on the classification of renal neoplasms recognized it as a specific entity and adopted the name “mucinous tubular and spindle cell carcinoma†(MTSCC). Although collecting duct epithelium is favored as site of origin, debate exists if it is actually of loop of Henle origin.
MTSCC is a rare renal neoplasm primarily of adult women. There is a 4:1 female predominance, with an average presentation of 53 years (range: 13 to 82) [Yang et al, Lima et al]. Typically asymptomatic, the tumor is commonly discovered incidentally while imaging for other reasons. But when the tumor is large it may present with flank pain or hematuria and consequential anemia.
Grossly, the tumor is well-circumscribed, gray-white, tan, or yellow and lacks significant hemorrhage or necrosis. Due to variable mucin content, cut surfaces may appear shiny or “mucoidâ€. It is usually 2.0 to 4.0 cm in size, although tumors less than 1.0 cm to greater than 18.0 cm have been described [Lima et al].
Microscopically, MTSCC consists of compact interconnecting tubules lined by bland low-cuboidal cells with eosinophilic, sometimes vacuolated cytoplasm. Samson, et al, noted vacuolization in 2 cases out of 17 analyzed. There are varying degrees of spindled cells arranged in cords, separated by pale basophilic myxoid stroma. “Mucin poor†variants are sometimes observed, where the spindled component becomes paramount for correct diagnosis [Rosai]. Of note, the spindled cells show low-grade round to oval nuclei, distinct from high-grade nuclei seen in sarcomatoid entities. Occasionally, focal neuroendocrine differentiation may be seen. Although not normally prominent; papillations, chronic inflammation, necrosis, and foam cells may be present. Phenotypically, the tumor cells characteristically express low molecular weight cytokeratins (CK7, CK19), EMA, AMACR, and vimentin. Generally, they do not express RCC, CD10, HMWCK, or CD117 [Ursani et al].
The differential diagnosis is fairly limited:
• Papillary renal cell carcinoma (PRCC) shows areas of compacted tubules and glomeruloid formations but usually lacks spindled cells and mucin. Thought to arise from proximal tubule origin, PRCC expresses CD10, unlike MTSCC.
• Sarcomatoid variant of renal cell carcinoma is a malignant neoplasm in which spindled cells characteristically display high grade cytology.
• Collecting duct carcinoma demonstrates small cysts and tubular structures but the lining cells are generally pleomorphic with high nuclear grades and a frequent hobnail morphology. Instead of having a mucinous background, the stroma of collecting duct carcinoma shows inflammation and desmoplasia.
Mucinous tubular and spindle cell carcinoma is a rare tumor only recently described as a distinct entity. Despite its pleomorphism and spindled morphology, it carries a better prognosis than other renal cell malignancies. Since it behaves less aggressively than other renal cell carcinomas, it is important to separate it from more common RCCs so that they may receive appropriately different treatment.
Suggested Reading:
MacLennan GT, Farrow GM, Bostwick DG. Low-grade collecting duct carcinoma of the kidney: report of 13 cases of low-grade mucinous tubulocystic renal carcinoma of possible collecting duct origin. Urology 1997; 50:679.
Lima et al.: The imaging and pathological features of a mucinous tubular and spindle cell carcinoma of the kidney: a case report. World J Surg Oncol 2013 11:34.
Gregory T. MacLennan GT, Bostwick DG. Tubulocystic Carcinoma, Mucinous Tubular and Spindle Cell Carcinoma, and Other Recently Described Rare Renal Tumors. Clin Lab Med 2005; 25(2): 393-416.
Rosai, J, Ackerman LV. Rosai and Ackerman’s Surgical Pathology. 10th ed. Mosby. 2004: Ch. 17. 1189.
Fine SW, Argani P, DeMarzo AM, Delahunt B, Sebo TJ, Reuter VE, Epstein JL. Expanding the Histologic Spectrum of Mucinous Tubular and Spindle Cell Carcinoma of the Kidney. Am J Surg Pathol 2006;30:1554-1560.
Yang G, Breyer BN, Weiss DA, MacLennan GT. J Urol. 2010 Feb;183(2):738-9.
Zhou M, Netto GJ, Epstein JI. Uropathology. Elsevier/Saunders. 2012: 287.